Cell Lung Cancer, Mesothelioma, And Thymoma
As examined in the Non-Small-Cell Lung Cancer" section, there are two noteworthy subdivisions of lung cancer: little cell lung cancer (SCLC) and non-little cell lung cancer (NSCLC). SCLC is diminishing in recurrence in the United States, with late information indicating it speaks to just 14% of lung cancers. This section gives data on the staging and visualization, pathology and pathophysiology, treatment, and follow-up of long haul survivors of SCLC and closes with brief dialogs on mesothelioma and thymoma.
The Non-Small-Cell Lung Cancer" part gives data on the study of disease transmission, etiology, screening and counteractive action, and determination of lung cancer all in all and spreads NSCLC and carcinoid tumors of the lungs.
Staging and Prognosis
A worldwide database comprising of 8,088 patients with SCLC was created by the International Association for the Study of Lung Cancer (IASLC). Their investigation demonstrated that the seventh version of the American Joint Committee on Cancer (AJCC) TNM staging framework is material to SCLC. The IASLC suggests that the seventh release of the AJCC rules for staging lung cancer ought to be connected to both NSCLC and SCLC (see Non-Small-Cell Lung Cancer" section, Table 1 ). SCLC has beforehand been portrayed as either restricted (M0) or broad (M1), despite the fact that these general terms are lacking while assessing the part of the surgery. Patients with SCLC who have stages I to III infection, barring those with a dangerous pleural emission, are named having restricted illness. These patients constitute around 33% of all SCLC patients. The rest of the SCLC patients fall into the broad sickness class, which incorporates any patient with a dangerous pleural emission or any site of far-off infection, for example, the mind, liver, adrenal organ, bone, and bone marrow.
The staging of lung cancer must be directed in a systematic and itemized way to allow proper restorative proposals and to permit correlation of treatment comes about because of various foundations.
The stage is generally revealed as either clinical or pathologic. The previous depends on noninvasive (or insignificantly obtrusive) tests, while the last depends on tissue acquired amid surgery (see Non-Small-Cell Lung Cancer" section).
The most imperative prognostic factor in lung cancer is the phase of sickness. Inside a given malady arrange, the following most essential prognostic elements are execution status and late weight reduction. The two scales used to characterize execution status are the Eastern Cooperative Oncology Group (ECOG) execution status framework and the Karnofsky execution list (see Appendix 1). So, patients who are wandering have an essentially longer survival. The individuals who have lost at least 5% of body weight amid the first 3 to a half year have a more regrettable guess.
Read Also : Know More About Lung Cancer
SCLC tends to give a huge focal lung mass and related broad hilar and mediastinal lymphadenopathy. Clinically obvious far off metastases are available in around 66% of patients at a conclusion. What's more, information from post-mortem examination demonstrates micrometastatic sickness in 63% of patients who passed on inside 30 days of endeavored therapeutic resection of SCLC. Hence, it is a foundational infection at introduction in the lion's share of patients.
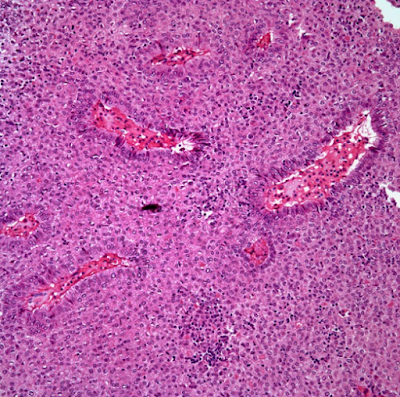
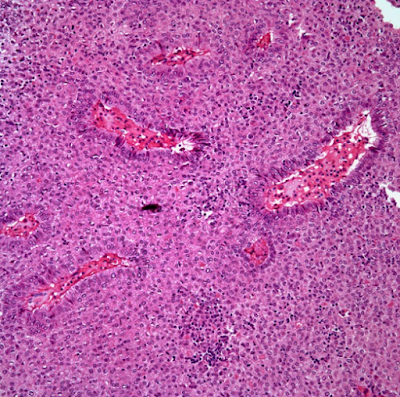
SCLC is a little, blue, round cell tumor that is primitive and undifferentiated at the light minuscule level. Electron microscopy exhibits its neuroendocrine determination by the nearness of thick center granules. The immunohistochemical proof of neuroendocrine determination incorporates positively recoloring for chromogranin, synaptophysin, and different proteins. The amine antecedent take-up and decarboxylation apparatus exhibit in the thick center granule prompts the generation of naturally dynamic amines and advances the blend of polypeptide hormones, for example, antidiuretic hormone (ADH) and adrenocorticotropic hormone (ACTH). Paraneoplastic disorders create because of hormone overabundance. The most widely recognized of these disorders, disorder of unseemly antidiuretic hormone emission (SIADH), happens in roughly 10% of patients with SCLC. Hypercortisolism and a Cushing-like disorder are more uncommon, seen in just 1% to 2% of patients.
Treatment of malady constrained to lung parenchyma
Surgery. The greater part of patients with SCLC gives propelled organize ailment. In the 5% to 10% of patients whose tumor is constrained to the lung parenchyma, regularly the determination is built up simply after the lung mass has been evacuated. Assuming, be that as it may, the histology has been dictated by bronchoscopic biopsy or fine-needle goal and there is no proof of metastatic sickness following broad checking, examination of the bone marrow, and biopsy of the mediastinal lymph hubs, at that point resection, ought to be performed. Adjuvant chemotherapy is prescribed due to the high probability of advancement of far-off metastases following surgery.
The surgical approach in SCLC is like that utilized as a part of NSCLC: A lobectomy or pneumonectomy ought to be trailed by an exhaustive mediastinal lymph hub dismemberment. In a current review contemplate by Tashi et al, patients with constrained stage SCLC who experienced surgical resection had enhanced middle survivals over all stages. Right now, in any case, tumor resection in SCLC ought to be restricted to patients who have no proof of mediastinal or supraclavicular lymph hub metastases. Information recommend that patients with SCLC exhibiting as a singular aspiratory knob and turned out to be arranged I have a 5-year survival rate of around 70% when treated with resection and adjuvant chemotherapy.
Treatment of disease limited to the thorax
Approximately one-third of SCLC patients present with disease that is limited to the thorax and can be encompassed within a tolerable radiation portal. In early studies in which either radiation therapy or surgery alone was used to treat such patients, median survival was only 3 to 4 months, and the 5-year survival rate was in the range of 1% to 2%. The reason for the failure of these therapies was both rapid recurrence of intrathoracic tumor and development of distant metastasis.
Chemotherapy. During the 1970s, it became apparent that SCLC was relatively sensitive to chemotherapy. Various combination chemotherapy regimens were used to treat limited SCLC. Although none of the regimens was clearly superior, median survival was approximately 12 months, and the 2-year survival rate was approximately 10% to 15%. It appears that maintenance chemotherapy adds little to survival in patients with limited SCLC.
Chemotherapy plus thoracic irradiation. One of the major advances in treating SCLC in the past 15 years is the recognition of the value of early and concurrent thoracic chemoradiation therapy. This advance was clearly facilitated by the increase in therapeutic index when PE (cisplatin Platinol/etoposide) chemotherapy is given with thoracic irradiation, as opposed to older anthracycline- or alkylator-based regimens. Although the major impact from this approach is improved locoregional tumor control, there are hints from randomized trials that early control of disease in the chest can also reduce the risk of distant metastasis.
An Intergroup trial directly compared once-daily vs twice-daily fractionation (45 Gy/25 fractions/5 weeks vs 45 Gy/30 fractions/3 weeks) given at the beginning of concurrent chemoradiation therapy with PE. Initial analysis showed excellent overall results, with median survival for all patients of 20 months and a 40% survival rate at 2 years. With a minimum follow-up of 5 years, survival was significantly better in the twice-daily than in the once-daily irradiation group (26% vs 16%). The main difference in toxicity was a temporary increase in grade 3 esophagitis in patients receiving twice-daily radiation therapy.
Outcomes for patients with limited-stage SCLC have improved significantly over the past 20 years. In an analysis of phase III trials during this period, median survival was 12 months in the control arm in 26 phase III studies initiated between 1972 and 1981, compared with 17 months in studies between 1982 and 1992 (P <001). Five studies demonstrated a statistically significant improvement in survival in the experimental arm compared with the control arm. Interestingly, all five studies involved some aspect of thoracic radiation therapy (three trials compared chemotherapy alone with chemoradiation therapy; one compared early radiation therapy with late radiation therapy; and one compared once-daily with twice-daily thoracic radiation therapy). Similarly, data from the Surveillance, Epidemiology, and End Results (SEER) database demonstrate that the 5-year survival rate has more than doubled from 1973 to 1996 (5.2% vs 12.2%; P =0001).
• Current recommendations—Although important questions remain as to the optimal radiation doses, volumes, and timing with regard to chemotherapy, a reasonable standard is to deliver thoracic irradiation concurrently with PE chemotherapy (cisplatin 60 mg/m2 IV on day 1 and etoposide 120 mg/ m2 IV on days 1 to 3). An attempt is made to integrate thoracic irradiation as early as possible, during cycle 1 (or 2).
Fried et al performed a meta-analysis evaluating early vs late timing of radiation therapy in limited-stage SCLC. Earlier radiation therapy was defined as that given prior to 9 weeks after initiation of chemotherapy vs late radiation therapy (≥ 9 weeks). Seven trials (N = 1,542 patients) were included in the analysis. They reported a small but significant improvement in 2-year overall survival for early vs late radiation therapy (5.2%; P =03). This finding is similar to the benefit of adding radiation therapy or prophylactic cranial irradiation (PCI) to chemotherapy. A greater difference was evident for the subset of patients receiving early rather than late hyperfractionated radiation therapy and platinum-based chemotherapy. Hyperfractionated accelerated fractionation should be considered, given the results of the Intergroup 0096 trial. An Intergroup phase III study is under way to compare twice-daily radiation therapy to 45 Gy, once-daily with radiation therapy to a higher dose (70 Gy), and a modified regimen combining these strategies (Radiation Therapy Oncology Group RTOG trial; ID NCT00632853).
Irradiation can be incorporated sequentially with chemotherapy; however, this approach appears to be inferior to early concurrent therapy and should be reserved for use in patients for whom concurrent
approaches are predicted to be excessively toxic.
A randomized trial of concurrent vs sequential thoracic radiotherapy in combination with PE in more than 200 patients with limited-stage SCLC (Takada et al: J Clin Oncol 2002) demonstrated a benefit to concurrent therapy, with a median survival of 27 months (30%, concurrent arm) vs 19.7 months (20%, sequential arm; P =097). Thoracic radiation therapy consisted of 45 Gy over 3 weeks, starting either with the first cycle of PE in the concurrent arm or after the fourth cycle in the sequential arm.
Komaki et al have reported both phase I and II data with a concomitant boost” chemoradiation approach (RTOG 0239). This therapy involved treating the initial large field in daily fractions and boosting the small field to a higher dose (61.2 Gy in 5 weeks), with a second daily fraction on the last 9 days of treatment. The chemotherapy regimen included etoposide and cisplatin. The locoregional tumor control rate at 2 years was 80%, although the 2-year survival rate of 37% was not as promising. Severe grade esophagitis occurred in 18% of patients, which is lower than the rate of 27% observed in the accelerated arm of Intergroup 0096.
Movsas et al reported the results of the first Patterns of Care Study (PCS) for lung cancer in the United States. This study was conducted to determine the national patterns of radiotherapy practice in patients treated for nonmetastatic lung cancer in 1998 and 1999. As supported by clinical trials, patients with limited-stage SCLC received chemotherapy plus radiotherapy more often than radiotherapy alone (92% vs 5%; P <001). However, only 6% of patients received hyperfractionated (twice-daily) radiotherapy. A total of 22% received PCI, with a median dose of 30 Gy in 15 fractions. Of note, in a more recent follow-up PCS/Quality Research in Radiation Oncology study by Komaki et al, the rate of twice-daily radiotherapy increased to about 20% and the rate of PCI use increased to about 50%.
Interestingly, in 2002 Choi et al (Proc Am Soc Clin Oncol) reported long-term survival data from their phase I trial assessing chemotherapy with either standard daily radiotherapy or accelerated twice-daily radiotherapy from the Cancer and Leukemia Group B (CALGB) 8837 trial. They previously reported that the maximum tolerated dose was 45 Gy in 30 fractions for twice-daily radiotherapy and more than 70 Gy in 35 fractions for once-daily radiotherapy. The 5-year survival estimated (from this phase I trial) for the twice-daily arm was 20%, vs 36% for the once-daily radiotherapy arm. There is currently a large Intergroup trial testing three chemoradiation regimens for limited-disease SCLC (CALGB 30610/RTOG 0538). This study includes the accelerated regimen from Intergroup 0096, the concomitant boost from RTOG 0239, and the daily conventional fractionation as studied by Choi et al, with etoposide and cisplatin in all three arms.
Kubota et al conducted a randomized phase III study to test the role of three cycles of irinotecan and cisplatin (IP) vs three cycles of etoposide and cisplatin (EP) following one cycle of EP with concurrent accelerated hyperfractionated radiotherapy (45 Gy/3 weeks) in patients with limited-stage SCLC. No survival advantage was demonstrated by using IP vs EP (with 5-year overall survival rates of 36% and 34%, respectively).
Surgery. Although surgical resection is not usually part of the standard therapy for SCLC, the Japanese Clinical Oncology Lung Cancer Study Group (JCOLCSG) reported the results of a phase II trial of postoperative adjuvant PE in patients with completely resected stages I to IIIA SCLC. The 5-year survival rates (in a cohort of 62 patients) for patients with pathologic stages I, II, and IIIA SCLC were 69%, 38%, and 40%, respectively.
The role of surgery for stage II or IIIA SCLC has evolved from a number of phase II trials and retrospective case series to include specific include resection of tumors with mixed histology (containing both SCLC and NSCLC components), salvage surgery for chemoresistant localized SCLC or local relapse after initial response to chemoradiotherapy, or second primary tumors after cure of initial SCLC. The rate of second primary NSCLC in patients treated for SCLC can be as high as 2% to greater than 10% per year (Johnson: J Natl Cancer Inst 1998).
Prospective randomized trials are ongoing in Europe and Japan to examine the role of surgery as part of multimodality therapy for patients with stages II and IIIA SCLC.
Recently, gene expression profiling has identified a subset of SCLC patients with good prognosis. A 2014 study by Hamanaka et al reported that low neuroendocrine marker expression, found mainly in SCLC patients who underwent surgical resection, was independently associated with prolonged survival.
Prophylactic cranial irradiation. Recognition that patients with SCLC are at high risk for development of brain metastases led to the suggestion that they be given PCI to prevent the clinical manifestation of previously present but occult CNS disease.
A meta-analysis of all randomized trials of PCI in patients with SCLC who achieved a complete or near-complete response to induction chemotherapy (alone or combined with thoracic irradiation) showed a statistically significant improvement in survival in patients treated with PCI (20.7% at 3 years vs 15.3% in those not given PCI). The survival improvement with PCI was seen in all patient subgroups, regardless of age, stage of disease, type of induction treatment, or performance status. Approximately 85% of the patients included in the meta-analysis had limited disease, and recommendations for use of PCI have been applied generally to this subgroup. One randomized trial, however, suggests benefit for PCI in patients with responding extensive disease as well.
Given the high incidence of symptomatic brain metastases and the relatively short survival following this event in patients with extensive SCLC, the European Organisation for Research and Treatment of Cancer (EORTC) randomized 286 patients after response to chemotherapy to receive PCI or not. Irradiation reduced the risk of symptomatic brain metastases, with a hazard ratio of 0.27 (95% CI, 0.16-0.44; P <001). The cumulative incidence of brain metastases was reduced from 40% in the control group to 15% within 1 year of follow-up. From the time of randomization, patients who were irradiated had an approximate 2-month increase in median survival (6.7 months vs 5.4 months) and double the 1-year survival rate (27% vs 13%); progression-free survival was less affected (14.7 weeks vs 12 weeks). PCI was reasonably well tolerated, with expected acute effects of headache, nausea and vomiting, and fatigue. Irradiated patients were more frequently given chemotherapy at the time of extracranial disease progression (68% vs 45%). Furthermore, only 59% of patients in the control group who developed brain metastases were treated with whole-brain irradiation. These latter factors may have contributed to the observed survival differences. Of note, brain imaging was not required for enrollment in this study.
A randomized trial reported by Le Péchoux et al in 2009 studied the issue of standard-dose vs higher-dose PCI in patients with limited-stage SCLC. Half of 720 patients with limited-stage SCLC in complete remission were randomly assigned to receive a standard-dose PCI regimen (25 Gy in 10 fractions). The other half received a higher PCI total dose (36 Gy) delivered using either conventional (18 daily fractions of 2 Gy) or accelerated hyperfractionated (24 fractions in 16 days of 1.5 Gy) radiation. With a median follow-up of 39 months, there was no significant difference in the 2-year incidence of brain metastases between the arms. The 2-year survival was 42% in the standard-dose group and 37% in the higher-dose group (P =05). The lower overall survival in the higher-dose group was thought to be due to an increase in cancer-related mortality. Overall, this randomized study showed no significant reduction in brain metastases after higher-dose PCI, but there was a significant increase in mortality. Therefore, standard doses of PCI should remain the standard of care in limited-stage SCLC. In reporting on RTOG 0212, Wolfson et al noted that 36 Gy delivered once or twice daily resulted in a greater risk of neurocognitive toxicity than did 25 Gy of PCI. Age greater than 60 years was significantly predictive for the possibility of this complication.
• Current recommendations—Patients should be offered PCI after completion of chemotherapy/chemoradiation therapy if they have clear regression of disease and a retained ECOG performance status of 0 to 2. Optimal integration of PCI should occur within 3 to 5 weeks of the last cycle of chemotherapy.
Radiation doses for PCI should be 25 to 30 Gy, with a daily fraction size of 2.5 to 2 Gy, respectively.
Treatment of extensive disease
As mentioned previously, two-thirds of SCLC patients have extensive disease at diagnosis. Without treatment, median survival in this group of patients is 6 to 8 weeks. Treatment with combination chemotherapy increases the median survival duration to approximately 8 to 10 months.
TABLE 1: Common chemotherapy regimens for SCLC
Induction chemotherapy. The combination of cisplatin or carboplatin/etoposide (see Table 1 for common dose ranges) is considered the standard of care in the United States at this time. This standard is primarily based on therapeutic index, because randomized trials have not demonstrated a survival benefit for this combination relative to the older regimen of cyclophosphamide, doxorubicin, and vincristine. The regimen is repeated at 3-week intervals for 4 to 6 courses. In North America, multiple randomized trials of newer cytotoxins replacing etoposide in a doublet with cisplatin, or added to the etoposide/platin base, have not provided a survival benefit. Japanese data that showed a 3.4-month survival advantage for irinotecan, as opposed to etoposide, with cisplatin were not confirmed in a trial in the United States, and the North American patients were less tolerant of the irinotecan.
The role of consolidative extracranial irradiation for patients with one to three sites of extensive SCLC is being studied in a randomized, phase II study (RTOG 0937) currently open to accrual. This research is based on an earlier randomized study (Jeremic et al: J Clin Oncol 1999) which indicated that adding consolidative radiation therapy to the treatment of the most favorable subset of patients with extensive SCLC led to improved survival compared with use of chemotherapy alone.
Another large North American study, Southwest Oncology Group (SWOG) S0124, and a trial from Germany comparing irinotecan with etoposide, when both are combined with platinating agents, were recently reported. Both showed equivalence in major efficacy outcomes. A Scandinavian trial with a similar design demonstrated a 1.4-month increase in the median survival rate for irinotecan-based treatment. However, these results are suspect because of an imbalance of elderly patients between the arms and a mandated dose reduction for etoposide in the elderly group. Overall, the data suggest that efficacy is equivalent with either approach. Because of problematic severe diarrhea with irinotecan, the therapeutic index may be improved with etoposide-based therapy.
Treatment of progressive disease
Progressive SCLC is classified on the basis of response and duration of response to initial induction therapy. Patients whose tumors do not regress or progress up to 60 to 90 days following the last cycle of chemotherapy are considered to have refractory disease. Conversely, patients whose tumors respond and who have an unmaintained progression-free interval longer than 60 to 90 days are deemed to have sensitive relapse. This categorization is based on the probability of objective response to additional cytotoxic therapy, which is uncommon, typically less than 15%, in the case of platin-refractory SCLC.
Topotecan is the only drug approved by the US Food and Drug Administration (FDA) for the treatment of recurrent disease. Its initial indication in 1998 was for patients with sensitive relapse and was based on similar efficacy compared with an older three-drug regimen. A subsequent trial compared IV administration with oral topotecan capsules, documenting similar efficacy and tolerance.
Most recently, a randomized trial compared oral topotecan with best supportive care in 141 patients with an ECOG performance status of 0 to 2. Patients with both refractory and sensitive disease were accrued. Median survival was nearly doubled on the topotecan arm, 26 weeks vs 14 weeks (P =0104), as was 6-month survival, 49% vs 26%. Benefit was seen in all subgroups analyzed, including patients with refractory cancer and an ECOG performance status of 2. Despite a low rate of response to topotecan of 7% and typical adverse effects, treated patients had slower deterioration of quality of life and improved symptom control. On the basis of these data, in October 2007 the FDA granted topotecan in capsule form a broad indication for treatment of recurrent SCLC.
More limited data with irinotecan suggest that its activity is probably similar to that of topotecan; however, it has never been evaluated in a randomized trial in the recurrent setting. Amrubicin, a synthetic anthracycline, has been studied extensively in recurrent SCLC in Japan and has been approved there. Initial data published in abstract form in North American patients suggest promising response rates with amrubicin in patients with refractory disease and a similar survival benefit as observed with topotecan in sensitive relapse. Amrubicin remains investigational in the United States.
Other cytotoxins, known more for their efficacy in NSCLC, such as docetaxel and paclitaxel, gemcitabine, and vinorelbine, do not have high single-agent response rates in therapy-naive SCLC and are not recognized as standard in management.
Integration of biologics in therapy. Ongoing clinical research is focused on integration of molecularly targeted therapy in an effort to make progress in treating this stubborn malignancy. At this time, data from completed trials do not indicate an active strategy with a biologic, whether in combination with induction chemotherapy, as maintenance following induction, or as single agents for recurrent disease.
• High-dose chemotherapy plus bone marrow transplant (BMT) —Most phase II trials using high doses of chemotherapy plus BMT appear to show no advantage to the high-dose approach over standard doses of chemotherapy.
• Alternating chemotherapy regimens—These have been used to overcome drug resistance. In randomized trials, alternating chemotherapy regimens have shown a slight improvement in terms of median survival (4 to 6 weeks) when compared with a single chemotherapeutic regimen, but no improvement in long-term survival.
Sidebar: In 2013 the American College of Radiology (ACR) published appropriateness criteria for the role of radiation therapy in SCLC. The ACR Appropriateness Criteria are evidence-based guidelines for specific clinical conditions. They are reviewed every 2 years by a multidisciplinary expert panel. The guideline development includes an extensive analysis of current medical literature and the application of a consensus methodology (modified Delphi) to rate the appropriateness of treatment recommendations by the panel. The SCLC topic provides an evidence-based approach regarding the role, dose, fractionation, technology, volume, and timing of thoracic radiation, as well as PCI in SCLC. The ACR Appropriateness Criteria also include discussions of other topics related to lung cancer and guidelines for patients with other types of cancer (Kong FM et al: Am J Clin Oncol 36:206-213, 2013).
Palliation of local and distant symptoms
Radiation therapy. Many patients with lung cancer have distressing local symptoms at some point in their disease course. These symptoms may arise from airway obstruction by the primary tumor, compression of mediastinal structures by nodal metastases, or metastatic involvement of distant organs. Radiation therapy is effective in palliating most local symptoms as well as symptoms at common metastatic sites, such as in bone and the brain.
In the United States, most radiation oncologists use doses in the vicinity of 30 Gy in 10 fractions for palliative treatment. Data from the United Kingdom suggest that similar efficacy without greater toxicity may be achieved with more abbreviated schedules, such as 17 Gy in two fractions 1 week apart or single fractions of 11 Gy (see Non-Small-Cell Lung Cancer” chapter, Table 8). Such schedules may facilitate the coordination of irradiation and chemotherapy, and they also may reduce patient travel and hospitalization.
Endobronchial irradiation with cobalt-60 or iridium-192 has been used to palliate symptoms arising from partial airway obstruction, including cough, dyspnea, and hemoptysis. The dosimetric advantage of being able to deliver a high radiation dose to the obstructing endobronchial tumor while sparing adjacent normal structures, such as the lungs, spinal cord, and esophagus, has clear appeal, particularly in the patient whose disease has recurred following prior external beam irradiation. Although good rates of palliation have been reported with endobronchial irradiation, significant complications, including fatal hemoptysis, are seen in 5% to 10% of patients. It remains unclear whether this represents a true treatment complication or symptoms related to the underlying disease.
Other local approaches. Endobronchial irradiation should be considered as only one of several approaches (including laser excision, cryotherapy, and stent placement) in the treatment of patients with symptomatic airway obstruction, and management should be individualized. All of these approaches are more suitable for partial than for complete airway obstruction.
Chemotherapy. Several trials have explored the use of chemotherapy to palliate specific symptoms in patients with lung cancer. In general, these trials have found that rates of symptomatic improvement were considerably higher than objective response rates and were not dissimilar to symptomatic response rates with local radiation therapy. Chemotherapy in the patient with newly diagnosed lung cancer is highly palliative for relief of symptoms related to superior vena cava syndrome, obstructive lung disease, and painful bony metastases. In the patient with recurrent disease, irradiation is more commonly associated with symptomatic relief of these localized problems. Radiation therapy remains the standard of care even for chemotherapy-naive patients with spinal cord compression or symptomatic brain metastasis.
The Non-Small-Cell Lung Cancer" part gives data on the study of disease transmission, etiology, screening and counteractive action, and determination of lung cancer all in all and spreads NSCLC and carcinoid tumors of the lungs.
Little Cell Lung Cancer
Staging and Prognosis
A worldwide database comprising of 8,088 patients with SCLC was created by the International Association for the Study of Lung Cancer (IASLC). Their investigation demonstrated that the seventh version of the American Joint Committee on Cancer (AJCC) TNM staging framework is material to SCLC. The IASLC suggests that the seventh release of the AJCC rules for staging lung cancer ought to be connected to both NSCLC and SCLC (see Non-Small-Cell Lung Cancer" section, Table 1 ). SCLC has beforehand been portrayed as either restricted (M0) or broad (M1), despite the fact that these general terms are lacking while assessing the part of the surgery. Patients with SCLC who have stages I to III infection, barring those with a dangerous pleural emission, are named having restricted illness. These patients constitute around 33% of all SCLC patients. The rest of the SCLC patients fall into the broad sickness class, which incorporates any patient with a dangerous pleural emission or any site of far-off infection, for example, the mind, liver, adrenal organ, bone, and bone marrow.
The staging of lung cancer must be directed in a systematic and itemized way to allow proper restorative proposals and to permit correlation of treatment comes about because of various foundations.
The stage is generally revealed as either clinical or pathologic. The previous depends on noninvasive (or insignificantly obtrusive) tests, while the last depends on tissue acquired amid surgery (see Non-Small-Cell Lung Cancer" section).
The most imperative prognostic factor in lung cancer is the phase of sickness. Inside a given malady arrange, the following most essential prognostic elements are execution status and late weight reduction. The two scales used to characterize execution status are the Eastern Cooperative Oncology Group (ECOG) execution status framework and the Karnofsky execution list (see Appendix 1). So, patients who are wandering have an essentially longer survival. The individuals who have lost at least 5% of body weight amid the first 3 to a half year have a more regrettable guess.
Read Also : Know More About Lung Cancer
Pathology and Pathophysiology
SCLC tends to give a huge focal lung mass and related broad hilar and mediastinal lymphadenopathy. Clinically obvious far off metastases are available in around 66% of patients at a conclusion. What's more, information from post-mortem examination demonstrates micrometastatic sickness in 63% of patients who passed on inside 30 days of endeavored therapeutic resection of SCLC. Hence, it is a foundational infection at introduction in the lion's share of patients.
SCLC is a little, blue, round cell tumor that is primitive and undifferentiated at the light minuscule level. Electron microscopy exhibits its neuroendocrine determination by the nearness of thick center granules. The immunohistochemical proof of neuroendocrine determination incorporates positively recoloring for chromogranin, synaptophysin, and different proteins. The amine antecedent take-up and decarboxylation apparatus exhibit in the thick center granule prompts the generation of naturally dynamic amines and advances the blend of polypeptide hormones, for example, antidiuretic hormone (ADH) and adrenocorticotropic hormone (ACTH). Paraneoplastic disorders create because of hormone overabundance. The most widely recognized of these disorders, disorder of unseemly antidiuretic hormone emission (SIADH), happens in roughly 10% of patients with SCLC. Hypercortisolism and a Cushing-like disorder are more uncommon, seen in just 1% to 2% of patients.
Treatment
Treatment of malady constrained to lung parenchyma
Surgery. The greater part of patients with SCLC gives propelled organize ailment. In the 5% to 10% of patients whose tumor is constrained to the lung parenchyma, regularly the determination is built up simply after the lung mass has been evacuated. Assuming, be that as it may, the histology has been dictated by bronchoscopic biopsy or fine-needle goal and there is no proof of metastatic sickness following broad checking, examination of the bone marrow, and biopsy of the mediastinal lymph hubs, at that point resection, ought to be performed. Adjuvant chemotherapy is prescribed due to the high probability of advancement of far-off metastases following surgery.
The surgical approach in SCLC is like that utilized as a part of NSCLC: A lobectomy or pneumonectomy ought to be trailed by an exhaustive mediastinal lymph hub dismemberment. In a current review contemplate by Tashi et al, patients with constrained stage SCLC who experienced surgical resection had enhanced middle survivals over all stages. Right now, in any case, tumor resection in SCLC ought to be restricted to patients who have no proof of mediastinal or supraclavicular lymph hub metastases. Information recommend that patients with SCLC exhibiting as a singular aspiratory knob and turned out to be arranged I have a 5-year survival rate of around 70% when treated with resection and adjuvant chemotherapy.
Treatment of disease limited to the thorax
Approximately one-third of SCLC patients present with disease that is limited to the thorax and can be encompassed within a tolerable radiation portal. In early studies in which either radiation therapy or surgery alone was used to treat such patients, median survival was only 3 to 4 months, and the 5-year survival rate was in the range of 1% to 2%. The reason for the failure of these therapies was both rapid recurrence of intrathoracic tumor and development of distant metastasis.
Chemotherapy. During the 1970s, it became apparent that SCLC was relatively sensitive to chemotherapy. Various combination chemotherapy regimens were used to treat limited SCLC. Although none of the regimens was clearly superior, median survival was approximately 12 months, and the 2-year survival rate was approximately 10% to 15%. It appears that maintenance chemotherapy adds little to survival in patients with limited SCLC.
Chemotherapy plus thoracic irradiation. One of the major advances in treating SCLC in the past 15 years is the recognition of the value of early and concurrent thoracic chemoradiation therapy. This advance was clearly facilitated by the increase in therapeutic index when PE (cisplatin Platinol/etoposide) chemotherapy is given with thoracic irradiation, as opposed to older anthracycline- or alkylator-based regimens. Although the major impact from this approach is improved locoregional tumor control, there are hints from randomized trials that early control of disease in the chest can also reduce the risk of distant metastasis.
An Intergroup trial directly compared once-daily vs twice-daily fractionation (45 Gy/25 fractions/5 weeks vs 45 Gy/30 fractions/3 weeks) given at the beginning of concurrent chemoradiation therapy with PE. Initial analysis showed excellent overall results, with median survival for all patients of 20 months and a 40% survival rate at 2 years. With a minimum follow-up of 5 years, survival was significantly better in the twice-daily than in the once-daily irradiation group (26% vs 16%). The main difference in toxicity was a temporary increase in grade 3 esophagitis in patients receiving twice-daily radiation therapy.
Outcomes for patients with limited-stage SCLC have improved significantly over the past 20 years. In an analysis of phase III trials during this period, median survival was 12 months in the control arm in 26 phase III studies initiated between 1972 and 1981, compared with 17 months in studies between 1982 and 1992 (P <001). Five studies demonstrated a statistically significant improvement in survival in the experimental arm compared with the control arm. Interestingly, all five studies involved some aspect of thoracic radiation therapy (three trials compared chemotherapy alone with chemoradiation therapy; one compared early radiation therapy with late radiation therapy; and one compared once-daily with twice-daily thoracic radiation therapy). Similarly, data from the Surveillance, Epidemiology, and End Results (SEER) database demonstrate that the 5-year survival rate has more than doubled from 1973 to 1996 (5.2% vs 12.2%; P =0001).
• Current recommendations—Although important questions remain as to the optimal radiation doses, volumes, and timing with regard to chemotherapy, a reasonable standard is to deliver thoracic irradiation concurrently with PE chemotherapy (cisplatin 60 mg/m2 IV on day 1 and etoposide 120 mg/ m2 IV on days 1 to 3). An attempt is made to integrate thoracic irradiation as early as possible, during cycle 1 (or 2).
Fried et al performed a meta-analysis evaluating early vs late timing of radiation therapy in limited-stage SCLC. Earlier radiation therapy was defined as that given prior to 9 weeks after initiation of chemotherapy vs late radiation therapy (≥ 9 weeks). Seven trials (N = 1,542 patients) were included in the analysis. They reported a small but significant improvement in 2-year overall survival for early vs late radiation therapy (5.2%; P =03). This finding is similar to the benefit of adding radiation therapy or prophylactic cranial irradiation (PCI) to chemotherapy. A greater difference was evident for the subset of patients receiving early rather than late hyperfractionated radiation therapy and platinum-based chemotherapy. Hyperfractionated accelerated fractionation should be considered, given the results of the Intergroup 0096 trial. An Intergroup phase III study is under way to compare twice-daily radiation therapy to 45 Gy, once-daily with radiation therapy to a higher dose (70 Gy), and a modified regimen combining these strategies (Radiation Therapy Oncology Group RTOG trial; ID NCT00632853).
Irradiation can be incorporated sequentially with chemotherapy; however, this approach appears to be inferior to early concurrent therapy and should be reserved for use in patients for whom concurrent
approaches are predicted to be excessively toxic.
A randomized trial of concurrent vs sequential thoracic radiotherapy in combination with PE in more than 200 patients with limited-stage SCLC (Takada et al: J Clin Oncol 2002) demonstrated a benefit to concurrent therapy, with a median survival of 27 months (30%, concurrent arm) vs 19.7 months (20%, sequential arm; P =097). Thoracic radiation therapy consisted of 45 Gy over 3 weeks, starting either with the first cycle of PE in the concurrent arm or after the fourth cycle in the sequential arm.
Komaki et al have reported both phase I and II data with a concomitant boost” chemoradiation approach (RTOG 0239). This therapy involved treating the initial large field in daily fractions and boosting the small field to a higher dose (61.2 Gy in 5 weeks), with a second daily fraction on the last 9 days of treatment. The chemotherapy regimen included etoposide and cisplatin. The locoregional tumor control rate at 2 years was 80%, although the 2-year survival rate of 37% was not as promising. Severe grade esophagitis occurred in 18% of patients, which is lower than the rate of 27% observed in the accelerated arm of Intergroup 0096.
Movsas et al reported the results of the first Patterns of Care Study (PCS) for lung cancer in the United States. This study was conducted to determine the national patterns of radiotherapy practice in patients treated for nonmetastatic lung cancer in 1998 and 1999. As supported by clinical trials, patients with limited-stage SCLC received chemotherapy plus radiotherapy more often than radiotherapy alone (92% vs 5%; P <001). However, only 6% of patients received hyperfractionated (twice-daily) radiotherapy. A total of 22% received PCI, with a median dose of 30 Gy in 15 fractions. Of note, in a more recent follow-up PCS/Quality Research in Radiation Oncology study by Komaki et al, the rate of twice-daily radiotherapy increased to about 20% and the rate of PCI use increased to about 50%.
Interestingly, in 2002 Choi et al (Proc Am Soc Clin Oncol) reported long-term survival data from their phase I trial assessing chemotherapy with either standard daily radiotherapy or accelerated twice-daily radiotherapy from the Cancer and Leukemia Group B (CALGB) 8837 trial. They previously reported that the maximum tolerated dose was 45 Gy in 30 fractions for twice-daily radiotherapy and more than 70 Gy in 35 fractions for once-daily radiotherapy. The 5-year survival estimated (from this phase I trial) for the twice-daily arm was 20%, vs 36% for the once-daily radiotherapy arm. There is currently a large Intergroup trial testing three chemoradiation regimens for limited-disease SCLC (CALGB 30610/RTOG 0538). This study includes the accelerated regimen from Intergroup 0096, the concomitant boost from RTOG 0239, and the daily conventional fractionation as studied by Choi et al, with etoposide and cisplatin in all three arms.
Kubota et al conducted a randomized phase III study to test the role of three cycles of irinotecan and cisplatin (IP) vs three cycles of etoposide and cisplatin (EP) following one cycle of EP with concurrent accelerated hyperfractionated radiotherapy (45 Gy/3 weeks) in patients with limited-stage SCLC. No survival advantage was demonstrated by using IP vs EP (with 5-year overall survival rates of 36% and 34%, respectively).
Surgery. Although surgical resection is not usually part of the standard therapy for SCLC, the Japanese Clinical Oncology Lung Cancer Study Group (JCOLCSG) reported the results of a phase II trial of postoperative adjuvant PE in patients with completely resected stages I to IIIA SCLC. The 5-year survival rates (in a cohort of 62 patients) for patients with pathologic stages I, II, and IIIA SCLC were 69%, 38%, and 40%, respectively.
The role of surgery for stage II or IIIA SCLC has evolved from a number of phase II trials and retrospective case series to include specific include resection of tumors with mixed histology (containing both SCLC and NSCLC components), salvage surgery for chemoresistant localized SCLC or local relapse after initial response to chemoradiotherapy, or second primary tumors after cure of initial SCLC. The rate of second primary NSCLC in patients treated for SCLC can be as high as 2% to greater than 10% per year (Johnson: J Natl Cancer Inst 1998).
Prospective randomized trials are ongoing in Europe and Japan to examine the role of surgery as part of multimodality therapy for patients with stages II and IIIA SCLC.
Recently, gene expression profiling has identified a subset of SCLC patients with good prognosis. A 2014 study by Hamanaka et al reported that low neuroendocrine marker expression, found mainly in SCLC patients who underwent surgical resection, was independently associated with prolonged survival.
Prophylactic cranial irradiation. Recognition that patients with SCLC are at high risk for development of brain metastases led to the suggestion that they be given PCI to prevent the clinical manifestation of previously present but occult CNS disease.
A meta-analysis of all randomized trials of PCI in patients with SCLC who achieved a complete or near-complete response to induction chemotherapy (alone or combined with thoracic irradiation) showed a statistically significant improvement in survival in patients treated with PCI (20.7% at 3 years vs 15.3% in those not given PCI). The survival improvement with PCI was seen in all patient subgroups, regardless of age, stage of disease, type of induction treatment, or performance status. Approximately 85% of the patients included in the meta-analysis had limited disease, and recommendations for use of PCI have been applied generally to this subgroup. One randomized trial, however, suggests benefit for PCI in patients with responding extensive disease as well.
Given the high incidence of symptomatic brain metastases and the relatively short survival following this event in patients with extensive SCLC, the European Organisation for Research and Treatment of Cancer (EORTC) randomized 286 patients after response to chemotherapy to receive PCI or not. Irradiation reduced the risk of symptomatic brain metastases, with a hazard ratio of 0.27 (95% CI, 0.16-0.44; P <001). The cumulative incidence of brain metastases was reduced from 40% in the control group to 15% within 1 year of follow-up. From the time of randomization, patients who were irradiated had an approximate 2-month increase in median survival (6.7 months vs 5.4 months) and double the 1-year survival rate (27% vs 13%); progression-free survival was less affected (14.7 weeks vs 12 weeks). PCI was reasonably well tolerated, with expected acute effects of headache, nausea and vomiting, and fatigue. Irradiated patients were more frequently given chemotherapy at the time of extracranial disease progression (68% vs 45%). Furthermore, only 59% of patients in the control group who developed brain metastases were treated with whole-brain irradiation. These latter factors may have contributed to the observed survival differences. Of note, brain imaging was not required for enrollment in this study.
A randomized trial reported by Le Péchoux et al in 2009 studied the issue of standard-dose vs higher-dose PCI in patients with limited-stage SCLC. Half of 720 patients with limited-stage SCLC in complete remission were randomly assigned to receive a standard-dose PCI regimen (25 Gy in 10 fractions). The other half received a higher PCI total dose (36 Gy) delivered using either conventional (18 daily fractions of 2 Gy) or accelerated hyperfractionated (24 fractions in 16 days of 1.5 Gy) radiation. With a median follow-up of 39 months, there was no significant difference in the 2-year incidence of brain metastases between the arms. The 2-year survival was 42% in the standard-dose group and 37% in the higher-dose group (P =05). The lower overall survival in the higher-dose group was thought to be due to an increase in cancer-related mortality. Overall, this randomized study showed no significant reduction in brain metastases after higher-dose PCI, but there was a significant increase in mortality. Therefore, standard doses of PCI should remain the standard of care in limited-stage SCLC. In reporting on RTOG 0212, Wolfson et al noted that 36 Gy delivered once or twice daily resulted in a greater risk of neurocognitive toxicity than did 25 Gy of PCI. Age greater than 60 years was significantly predictive for the possibility of this complication.
• Current recommendations—Patients should be offered PCI after completion of chemotherapy/chemoradiation therapy if they have clear regression of disease and a retained ECOG performance status of 0 to 2. Optimal integration of PCI should occur within 3 to 5 weeks of the last cycle of chemotherapy.
Radiation doses for PCI should be 25 to 30 Gy, with a daily fraction size of 2.5 to 2 Gy, respectively.
Treatment of extensive disease
As mentioned previously, two-thirds of SCLC patients have extensive disease at diagnosis. Without treatment, median survival in this group of patients is 6 to 8 weeks. Treatment with combination chemotherapy increases the median survival duration to approximately 8 to 10 months.
TABLE 1: Common chemotherapy regimens for SCLC
Induction chemotherapy. The combination of cisplatin or carboplatin/etoposide (see Table 1 for common dose ranges) is considered the standard of care in the United States at this time. This standard is primarily based on therapeutic index, because randomized trials have not demonstrated a survival benefit for this combination relative to the older regimen of cyclophosphamide, doxorubicin, and vincristine. The regimen is repeated at 3-week intervals for 4 to 6 courses. In North America, multiple randomized trials of newer cytotoxins replacing etoposide in a doublet with cisplatin, or added to the etoposide/platin base, have not provided a survival benefit. Japanese data that showed a 3.4-month survival advantage for irinotecan, as opposed to etoposide, with cisplatin were not confirmed in a trial in the United States, and the North American patients were less tolerant of the irinotecan.
The role of consolidative extracranial irradiation for patients with one to three sites of extensive SCLC is being studied in a randomized, phase II study (RTOG 0937) currently open to accrual. This research is based on an earlier randomized study (Jeremic et al: J Clin Oncol 1999) which indicated that adding consolidative radiation therapy to the treatment of the most favorable subset of patients with extensive SCLC led to improved survival compared with use of chemotherapy alone.
Another large North American study, Southwest Oncology Group (SWOG) S0124, and a trial from Germany comparing irinotecan with etoposide, when both are combined with platinating agents, were recently reported. Both showed equivalence in major efficacy outcomes. A Scandinavian trial with a similar design demonstrated a 1.4-month increase in the median survival rate for irinotecan-based treatment. However, these results are suspect because of an imbalance of elderly patients between the arms and a mandated dose reduction for etoposide in the elderly group. Overall, the data suggest that efficacy is equivalent with either approach. Because of problematic severe diarrhea with irinotecan, the therapeutic index may be improved with etoposide-based therapy.
Treatment of progressive disease
Progressive SCLC is classified on the basis of response and duration of response to initial induction therapy. Patients whose tumors do not regress or progress up to 60 to 90 days following the last cycle of chemotherapy are considered to have refractory disease. Conversely, patients whose tumors respond and who have an unmaintained progression-free interval longer than 60 to 90 days are deemed to have sensitive relapse. This categorization is based on the probability of objective response to additional cytotoxic therapy, which is uncommon, typically less than 15%, in the case of platin-refractory SCLC.
Topotecan is the only drug approved by the US Food and Drug Administration (FDA) for the treatment of recurrent disease. Its initial indication in 1998 was for patients with sensitive relapse and was based on similar efficacy compared with an older three-drug regimen. A subsequent trial compared IV administration with oral topotecan capsules, documenting similar efficacy and tolerance.
Most recently, a randomized trial compared oral topotecan with best supportive care in 141 patients with an ECOG performance status of 0 to 2. Patients with both refractory and sensitive disease were accrued. Median survival was nearly doubled on the topotecan arm, 26 weeks vs 14 weeks (P =0104), as was 6-month survival, 49% vs 26%. Benefit was seen in all subgroups analyzed, including patients with refractory cancer and an ECOG performance status of 2. Despite a low rate of response to topotecan of 7% and typical adverse effects, treated patients had slower deterioration of quality of life and improved symptom control. On the basis of these data, in October 2007 the FDA granted topotecan in capsule form a broad indication for treatment of recurrent SCLC.
More limited data with irinotecan suggest that its activity is probably similar to that of topotecan; however, it has never been evaluated in a randomized trial in the recurrent setting. Amrubicin, a synthetic anthracycline, has been studied extensively in recurrent SCLC in Japan and has been approved there. Initial data published in abstract form in North American patients suggest promising response rates with amrubicin in patients with refractory disease and a similar survival benefit as observed with topotecan in sensitive relapse. Amrubicin remains investigational in the United States.
Other cytotoxins, known more for their efficacy in NSCLC, such as docetaxel and paclitaxel, gemcitabine, and vinorelbine, do not have high single-agent response rates in therapy-naive SCLC and are not recognized as standard in management.
Integration of biologics in therapy. Ongoing clinical research is focused on integration of molecularly targeted therapy in an effort to make progress in treating this stubborn malignancy. At this time, data from completed trials do not indicate an active strategy with a biologic, whether in combination with induction chemotherapy, as maintenance following induction, or as single agents for recurrent disease.
• High-dose chemotherapy plus bone marrow transplant (BMT) —Most phase II trials using high doses of chemotherapy plus BMT appear to show no advantage to the high-dose approach over standard doses of chemotherapy.
• Alternating chemotherapy regimens—These have been used to overcome drug resistance. In randomized trials, alternating chemotherapy regimens have shown a slight improvement in terms of median survival (4 to 6 weeks) when compared with a single chemotherapeutic regimen, but no improvement in long-term survival.
Sidebar: In 2013 the American College of Radiology (ACR) published appropriateness criteria for the role of radiation therapy in SCLC. The ACR Appropriateness Criteria are evidence-based guidelines for specific clinical conditions. They are reviewed every 2 years by a multidisciplinary expert panel. The guideline development includes an extensive analysis of current medical literature and the application of a consensus methodology (modified Delphi) to rate the appropriateness of treatment recommendations by the panel. The SCLC topic provides an evidence-based approach regarding the role, dose, fractionation, technology, volume, and timing of thoracic radiation, as well as PCI in SCLC. The ACR Appropriateness Criteria also include discussions of other topics related to lung cancer and guidelines for patients with other types of cancer (Kong FM et al: Am J Clin Oncol 36:206-213, 2013).
Palliation of local and distant symptoms
Radiation therapy. Many patients with lung cancer have distressing local symptoms at some point in their disease course. These symptoms may arise from airway obstruction by the primary tumor, compression of mediastinal structures by nodal metastases, or metastatic involvement of distant organs. Radiation therapy is effective in palliating most local symptoms as well as symptoms at common metastatic sites, such as in bone and the brain.
In the United States, most radiation oncologists use doses in the vicinity of 30 Gy in 10 fractions for palliative treatment. Data from the United Kingdom suggest that similar efficacy without greater toxicity may be achieved with more abbreviated schedules, such as 17 Gy in two fractions 1 week apart or single fractions of 11 Gy (see Non-Small-Cell Lung Cancer” chapter, Table 8). Such schedules may facilitate the coordination of irradiation and chemotherapy, and they also may reduce patient travel and hospitalization.
Endobronchial irradiation with cobalt-60 or iridium-192 has been used to palliate symptoms arising from partial airway obstruction, including cough, dyspnea, and hemoptysis. The dosimetric advantage of being able to deliver a high radiation dose to the obstructing endobronchial tumor while sparing adjacent normal structures, such as the lungs, spinal cord, and esophagus, has clear appeal, particularly in the patient whose disease has recurred following prior external beam irradiation. Although good rates of palliation have been reported with endobronchial irradiation, significant complications, including fatal hemoptysis, are seen in 5% to 10% of patients. It remains unclear whether this represents a true treatment complication or symptoms related to the underlying disease.
Other local approaches. Endobronchial irradiation should be considered as only one of several approaches (including laser excision, cryotherapy, and stent placement) in the treatment of patients with symptomatic airway obstruction, and management should be individualized. All of these approaches are more suitable for partial than for complete airway obstruction.
Chemotherapy. Several trials have explored the use of chemotherapy to palliate specific symptoms in patients with lung cancer. In general, these trials have found that rates of symptomatic improvement were considerably higher than objective response rates and were not dissimilar to symptomatic response rates with local radiation therapy. Chemotherapy in the patient with newly diagnosed lung cancer is highly palliative for relief of symptoms related to superior vena cava syndrome, obstructive lung disease, and painful bony metastases. In the patient with recurrent disease, irradiation is more commonly associated with symptomatic relief of these localized problems. Radiation therapy remains the standard of care even for chemotherapy-naive patients with spinal cord compression or symptomatic brain metastasis.